Puberty vs. Adulthood: The Best Age for Gynecomastia Surgery
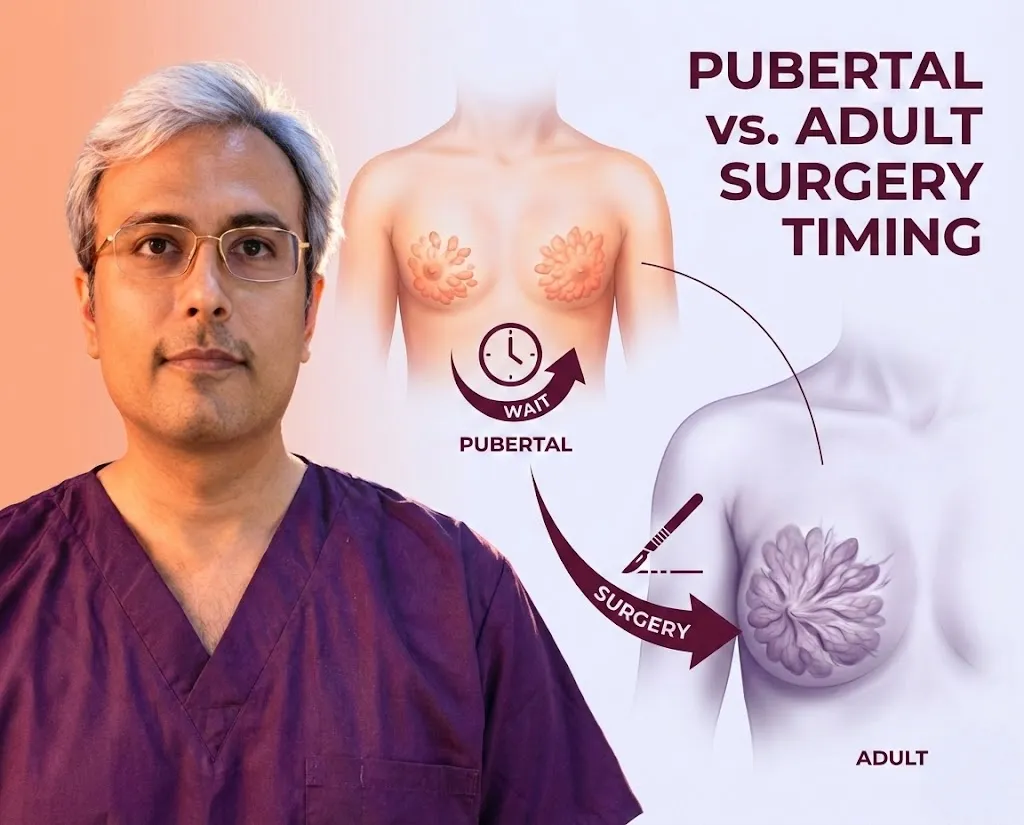
Pubertal Gynecomastia vs. Adult Gynecomastia: Should You Wait for Surgery?
For a teenage boy, few things are more distressing than noticing his chest is starting to look like a woman’s. It often leads to hunching over to hide the chest, avoiding swimming pools, and refusing to change in locker rooms. For parents, it is a confusing time: Is this just “baby fat” that will go away, or is it a permanent medical condition?
On the other hand, for adult men who have lived with enlarged breasts for years, the question isn’t “will it go away?” (spoiler: it usually won’t), but rather “is it too late to fix it?”
The approach to treating gynecomastia differs significantly depending on the patient’s age. While teenagers are often advised to wait, adults are encouraged to act.
In this guide, we will break down the biological differences between pubertal and adult gynecomastia, helping you decide whether to schedule a surgery or practice patience.
Understanding Pubertal Onset
Puberty is a hormonal rollercoaster. As a boy’s body transforms into a man’s, his hormone levels fluctuate wildly.
The “Growth Spurt” Hormone Storm
During early puberty (ages 12-14), the production of estrogen (the female hormone) often spikes before testosterone levels can catch up to balance it out. This temporary dominance of estrogen stimulates the breast tissue to grow.
Why 60% of Boys Get It
If you or your son is experiencing this, know that you are not alone. Studies show that up to 60% of adolescent boys develop some degree of transient gynecomastia. It is a physiological adaptation, not necessarily a disease.
Unsure if it is true glandular growth or just weight gain? Learn to spot the specific symptoms of onset to tell the difference.
Spontaneous Regression: The 2-Year Rule
The most important fact for parents to know is this: Most pubertal gynecomastia goes away on its own.
- As testosterone levels surge in late puberty (ages 15-17), the breast tissue typically shrinks and disappears.
- We generally follow the “2-Year Rule”: If the condition appeared recently, we wait at least two years to see if it resolves naturally before considering surgical intervention.
The Wait-and-See Approach
“Watchful waiting” doesn’t mean ignoring the problem. It means actively monitoring the condition while supporting the teenager’s mental health.
- Monitoring Size and Pain: Take photos every 3 months to track changes. If the breast buds are tender or painful, this is actually a good sign—it means the tissue is active and may regress as hormones stabilize.
- When to Consult an Endocrinologist: If the onset is very rapid, happens before age 10, or is accompanied by other symptoms (like headaches or vision changes), you should see a hormone specialist to rule out underlying issues like tumors.
- Psychological Impact: Pay attention to behavior. Is he withdrawing socially? Is he wearing hoodies in summer? The mental scar of bullying can last longer than the physical condition.
When to Operate on Teenagers
While we prefer to wait, there are exceptions. Surgery is sometimes recommended for teenagers under specific circumstances:
- Simon Grade 3 or 4: If the breasts are fully developed (female-looking cup size) with significant skin excess, they are unlikely to regress completely on their own. The skin has been stretched too far to snap back naturally.
- Severe Bullying and Mental Health Decline: If the condition is causing severe depression, anxiety, or school refusal, the benefits of surgery (improving quality of life) outweigh the risks of early operation.
- Stable Breast Size: We rarely operate if the breasts are actively growing. We look for a history of stable size for at least 12 months to ensure the condition has plateaued.
Adult Gynecomastia Characteristics
If you are over 20 and still have enlarged breasts, the “wait and see” period is over.
Why It Rarely Goes Away After 20
In adults, the glandular tissue changes. What was once soft and active becomes fibrotic (scar-like) and hard. Once this fibrosis sets in, no amount of diet, exercise, or “hormone balancing” will dissolve it. It must be physically removed.
Accumulated Fibrous Tissue vs. New Gland
Adult gynecomastia is often a mix of old, fibrotic gland from puberty and new fatty deposits from aging. This “mixed” tissue is tough and rubbery, requiring specialized surgical techniques to remove effectively.
Skin Elasticity in Older Patients
Teenagers have amazing skin elasticity—their skin snaps back tight after tissue removal. Adults, especially those over 30 or 40, have less collagen.
- This means older patients are at higher risk for loose skin post-surgery.
- They often have distinct skin tightening needs, sometimes requiring technologies like Renuvion or even skin excision lifts that teenagers rarely need.
Parental Guide to Surgery
If you are a parent considering this for your son, here is the logistical reality:
- Consent and Legal Age: In India, a patient under 18 cannot consent to surgery alone. Parents or legal guardians must sign all medical forms.
- Recovery Support for Students: The best time for teenage surgery is during school holidays (summer or winter break). This allows for the 1-2 weeks of downtime needed without missing classes or carrying heavy backpacks.
- Managing Expectations: Teens often expect “superhero” chests immediately. It is crucial to have a frank discussion about scars, the recovery timeline, and the need to wear a compression vest 24/7.
Conclusion
The decision to operate depends on the clock. For teenagers, patience is the prescription—give nature a chance to correct the imbalance. For adults, action is the answer—the condition is permanent unless treated.
Whether you are a concerned parent or an adult ready to reclaim your confidence, the first step is a professional evaluation to determine the maturity of the gland.
Is it time to act or time to wait? Contact Dr. Vishal Purohit for an honest assessment of your (or your son’s) condition. We prioritize the long-term physical and emotional health of our patients above all else.
Call or WhatsApp: +91 77181 83535