Gynecomastia Surgery Explained: Liposuction vs. Gland Excision
Gynecomastia Surgery Explained: Liposuction vs. Gland Excision
For many men suffering from enlarged breasts, the confusion isn’t just about why it’s happening, but how to fix it. If you’ve spent hours researching “male breast reduction,” you’ve likely encountered two distinct terms: Liposuction and Gland Excision.
Are they the same thing? Do you choose one over the other?
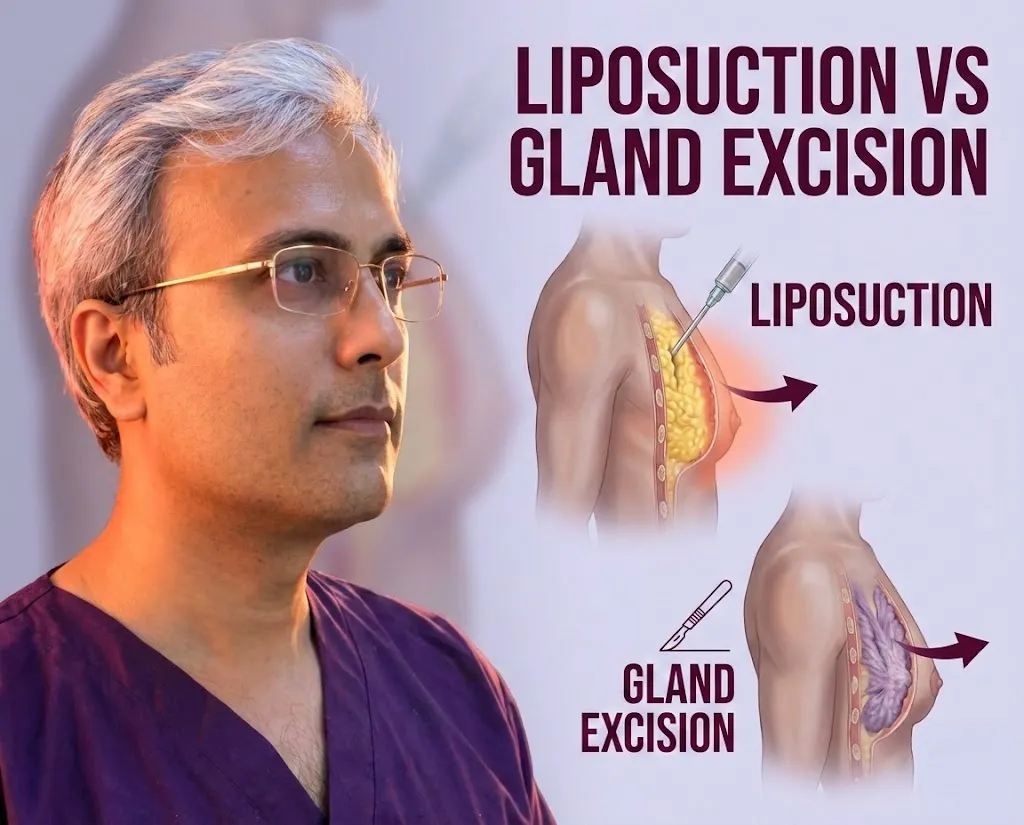
The short answer is: Gynecomastia surgery is rarely a single procedure. It is often a combination of techniques tailored to your specific anatomy. While liposuction removes the fatty tissue that creates bulk, gland excision removes the rubbery, fibrous disc directly behind the nipple that refuses to budge with diet and exercise.
In this guide, we will break down the differences between these techniques, how they work together, and which approach is right for your chest contouring goals.
The Two Components of Male Breast Reduction
To achieve a flat, masculine chest, a surgeon must address the two types of tissue that contribute to gynecomastia: adipose tissue (fat) and glandular tissue.
1. Addressing the Fat (Liposuction)
Many cases of gynecomastia, particularly pseudogynecomastia, consist largely of excess chest fat. This fat is soft, squishy, and can often be reduced—though not entirely eliminated—through weight loss. Liposuction is the gold standard for removing this fatty layer to contour the chest wall and armpit area.
2. Addressing the Gland (Excision)
True gynecomastia involves the proliferation of glandular tissue. Unlike fat, this tissue is firm, rubbery, and fibrous. It feels like a disc or a knot directly under the areola. Liposuction cannot remove this tissue; it is too dense to be sucked out through a cannula. It must be physically cut out (excised) to flatten the nipple area.
Why Most Patients Need Both
The most successful outcomes typically come from a combination approach.
- Liposuction is used first to “de-bulk” the chest and taper the edges so there are no harsh lines.
- Gland Excision follows to remove the dense core beneath the nipple.
If a surgeon performs only liposuction on a patient with true gland enlargement, the chest may look smaller, but the puffy nipple will remain, leading to an “unfinished” look.
Liposuction Techniques
Not all liposuction is created equal. Modern gynecomastia surgery utilizes advanced technologies to break down fat before removal, ensuring smoother results and less trauma to the body.
- Traditional Tumescent Liposuction: The surgeon injects a solution (saline, epinephrine, and lidocaine) to numb the area and shrink blood vessels. A cannula is then moved back and forth to manually break up and suction out the fat.
- VASER (Ultrasound-Assisted) Liposuction: This is a game-changer for male chest contouring. VASER uses ultrasound energy to liquefy fat cells specifically, leaving surrounding nerves and blood vessels intact. This allows for high-definition sculpting, etching out the pectoral muscle borders.
- Power-Assisted Liposuction (PAL): This technique uses a vibrating cannula. The rapid vibrations help the surgeon move through dense fibrous fat more easily, which is common in the male chest, reducing surgery time and recovery pain.
Ideal Candidate for Lipo-Only: Men who have pseudogynecomastia (mostly fat, no palpable gland) and good skin elasticity are the only candidates who might get away with liposuction alone.
Surgical Gland Excision
When the “puffy nipple” appearance persists, surgical excision is mandatory. This part of the procedure requires precision to ensure the nipple remains flat but alive.
The Webster Incision (Periareolar)
The standard technique involves a small, semi-circular incision made along the lower border of the areola (the dark skin surrounding the nipple). This placement is strategic because the scar eventually blends into the natural transition of pigment, becoming nearly invisible.
Removing the Fibrous Disc
Through this small opening, the surgeon dissects the glandular tissue away from the skin and muscle. The goal is to remove the bulk of the gland that is pushing the nipple outward.
Contouring the Areola and Minimizing “Craters”
One critical aspect of excision is avoiding a “crater deformity” or a sunken nipple. If a surgeon removes 100% of the tissue directly under the nipple, the nipple can adhere to the muscle, creating a divot when you flex.
- Experienced surgeons leave a tiny, thin layer of tissue (a few millimeters) attached to the nipple to maintain blood supply and ensure it sits flush with the chest.
- This technique is crucial for preventing regrowth while maintaining a natural look.
Skin Tightening Procedures
For Grade 1 and 2 gynecomastia, the skin naturally retracts after the fat and gland are removed. However, for Grade 3 and 4 cases (significant drooping), skin laxity is a major concern.
When Skin Excision is Necessary
If the breast has significant sagging (ptosis), simply removing the volume will leave an empty, hanging skin sac. In these severe cases, a surgeon may need to remove excess skin. This often results in a larger scar, sometimes around the entire areola (donut lift) or horizontally across the chest.
Radiofrequency Tightening (BodyTite/Renuvion)
For moderate skin laxity, surgeons can use minimally invasive Radiofrequency (RF) energy. Devices like BodyTite or Renuvion are inserted under the skin to heat the collagen network, causing it to contract and tighten (“shrink wrap”) over the muscle. This can often save a patient from needing large skin-removal incisions.
Note on Trade-offs: There is always a balance between achieving a perfectly flat chest and minimizing visible scarring. Understanding scar placement options is vital before agreeing to skin excision.
Anesthesia and Setting
The setting of your surgery often dictates the cost and the recovery experience.
- Local Anesthesia (Twilight Sedation): Many gynecomastia surgeries can be performed under local anesthesia with oral sedation. You are awake but relaxed and numb. This avoids the grogginess of general anesthesia and allows for a quicker discharge.
- General Anesthesia: For more complex cases involving large skin excision or anxious patients, general anesthesia (fully asleep) is preferred to ensure safety and comfort.
- In-Office vs. Surgery Center: Performing the procedure in an accredited in-office operating room can significantly lower the price by avoiding hospital facility fees. However, safety protocols must never be compromised.
Understanding how these choices affect your bill? Check out our guide on facility fees impact on cost.
Conclusion
Gynecomastia surgery is not a “one size fits all” procedure. It is a highly customized combination of liposuction to contour the chest wall and gland excision to flatten the nipple. Whether you need VASER technology for high-definition results or a simple gland removal depends entirely on your unique anatomy.
The first step to a flatter, more confident chest is a proper diagnosis to determine if you have fat, gland, or both.
Ready to define your chest? Contact Dr. Vishal Purohit today to schedule your consultation. We are here to guide you through every step of the transformation. Call or WhatsApp: +91 77181 83535